Perspectives
Growing the Open Dialogue Network with schools, services and communities.
The Open Dialogue Centre is a unique purpose-driven organisation established with the support of philanthropy to enable the widespread adoption of Open Dialogue.
Save the date! One Year Foundation Course in Melbourne
Location:
Docklands, Victoria
Dates:
Block 1 18-22nd August
Block 2 24-28 November
Block 3 16-20 Feb 2026
Block 4 27 Apr -1 May 2026
If you or someone you know is interested in how the Open Dialogue approach can complement and strengthen your way of working, our One Year Foundation Course will be delivered in four blocks throughout the year and is designed to provide mental health and wellbeing professionals with a framework to practice care that is truly person-centred and aligned with the World Health Organisation’s priorities.
This includes providing your communities with support that honours a person’s rights and includes their family, friends and social networks. The course will also support those who want to deepen their commitment to care and recovery- oriented pathways and the role of people with lived experience.
The training will incorporate engagement with the theory and principles of Open Dialogue and include participation in reflective practice and supervision, particularly around how social network meetings are facilitated.
The opportunity to participate in a community of practice will also be available to enable peer-learning, the sharing of experiences and access to the Centre’s growing evidence-base as we support the implementation of Open Dialogue around Australia.

Late last year I received an email from a GP in our network who is working in NSW.
He had taken the time to carefully synthesise the World Health Organisation’s (WHO) Community Guidance on mental health services which highlights examples from around the world where communities, services, hospitals, networks, homes, institutions and support groups are collaborating with people and families in innovative and inspiring ways. They are driving change in how mental health care is thought about and delivered.
A key point in his letter was the realisation that while Finland, Kenya, Brazil, Burma and many other regions all have solid stories of success with community-based and recovery-focused mental health care that respects people’s agency and rights, sadly, Australia has not been included in this publication with any examples.
The words ‘broken’ and ‘crisis’ are now regularly attached to descriptions of Australia’s mental health system across a growing number of reports, reviews and mainstream media articles. There is more than room for improvement. But more of the same solutions simply scaled up is clearly not going to shift the dial.
You can’t fix something by making it larger. You have to change it.

Professor Allan Fels was quoted in the Australian late last year (Dec 6th) as saying ‘Despite heroic efforts by countless individuals, the overall system of mental health is in crisis everywhere and at every level, for all ages and for all levels of intensity, from mild to severe, but especially for persons at the severe end.’
And as I read the recently published ANU report (with The Australian) Don’t Walk By I am struck by this summation:
‘The findings from all these comprehensive reviews…paint a picture of a national system for Australians that is overwhelmed, poorly coordinated, under-resourced, and not responsive to the needs of hundreds of thousands of people and their families. A system operating in crisis mode.’
The problems across our mental health system are well documented, but we also have a growing evidence-base that supports a very different way of working in mental health. This excites me in my role as CEO of Open Dialogue Centre and also in the work I’ve been involved in with over 20 years with young people experiencing homelessness.
It is my hope that through ODC’s network and this blog forum we can start raising awareness and having conversations about what we could do to change the system by doing things differently and leveraging a new evidence-base that supports the aspiration of those who work in mental health and wellbeing – from youth and mental health services to schools and communities – to create the conditions for people to thrive.
The World Health Organisation outlines a clear objective (in its mental health plan):
To provide comprehensive, integrated and responsive mental health and social care services in community-based settings.
We know that most people’s mental health is impacted by what is going on in their lives – factors that need to be addressed in a way that involves strategies for listening, learning, recovery, compassionate care, reducing stigma, and promoting early identification and prevention pathways. But implementing ways to honor these principles is challenging when the system is in crisis. Leaders may think there is no room to innovate and trial new approaches. The workforce gets burnt out because they are not supported to provide responses that are truly person-centered and rights-based.

In its 2013-2030 plan WHO defines health as ‘A state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.”
For the last three years, the Open Dialogue Centre has been meeting and working with people in mental health services, communities and schools to develop and strengthen the role that community networks can play in mental health care – meaning families, carers, friends, schools and services can work in coordinated and compassionate ways so that people have culturally safe and trusted environments to access support – when and where they need it, and before the crisis hits.
‘It needs to encompass a recovery-based approach that puts the emphasis on supporting individuals… to achieve their own aspirations and goals. The core service requirements include: listening and responding to individuals’ understanding of their condition and what helps them to recover; working with people as equal partners in their care; offering choice of treatment and therapies, and in terms of who provides care; and the use of peer workers and supports, who provide each other with encouragement and a sense of belonging, in addition to their expertise. In addition, a multisectoral approach is required whereby services support individuals, at different stages of the life-course and, as appropriate, facilitate their access to human rights such as employment (including return-to-work programmes), housing and educational opportunities and participation in community activities, programmes and meaningful activities.’
World Health Organisation, Comprehensive Mental Health Action Plan, 2013-2030
I have no doubt that soon we will be describing evidenced-based examples of community-based mental healthcare in Australia, using Open Dialogue as a way to prise open the potential for change and then enable communities to see it through.
WHO has a clear target for 80% of countries to have doubled the number of community-based mental health facilities, by 2030. Let’s make sure Australia is right there.

Open Dialogue has been around for 40 years. Why have we not seen widespread adoption?
Interest in the approach has been sustained and continues to grow but Open Dialogue has not become a mainstream service, and this is what the Open Dialogue Centre is committed to enabling.
It is why we are taking a systemic approach which means we will focus on creating the conditions in communities, organisations and service settings for Open Dialogue to thrive.
Snapshot: Building the evidence-base for Open Dialogue
The Open Dialogue Centre’s purpose is to enable the widespread adoption of Open Dialogue.
We are committed to an evidence-informed approach to trial, test, learn and grow Open Dialogue in priority settings including schools, mental health and youth services and communities around Australia.
There are some exciting things emerging in the coming months that will help us to strengthen the evidence-base for Open Dialogue in Australia:
1. The results of the ODDESSI trial will be released soon – ODDESSI is a large randomised control trial currently underway in the UK, researching the effectiveness of Open Dialogue in crisis and continuing metal health care within the National Health Service in the UK.
2. We are working with researchers from the University of Melbourne to review the evidence of Open Dialogue around the world.
3. We have engaged Clear Horizon to develop an outcomes measurement framework that will enable a consistent approach to demonstrating outcomes of Open Dialogue across the settings we are working in.
All of this is underpinned by learning cycles with partners and collaborators that allow us to reflect and adapt in real time to insights and evidence that are being generated on the ground.
Our approach to learning will also include engagement with young people as part of the co-design and adaptation of the approach.
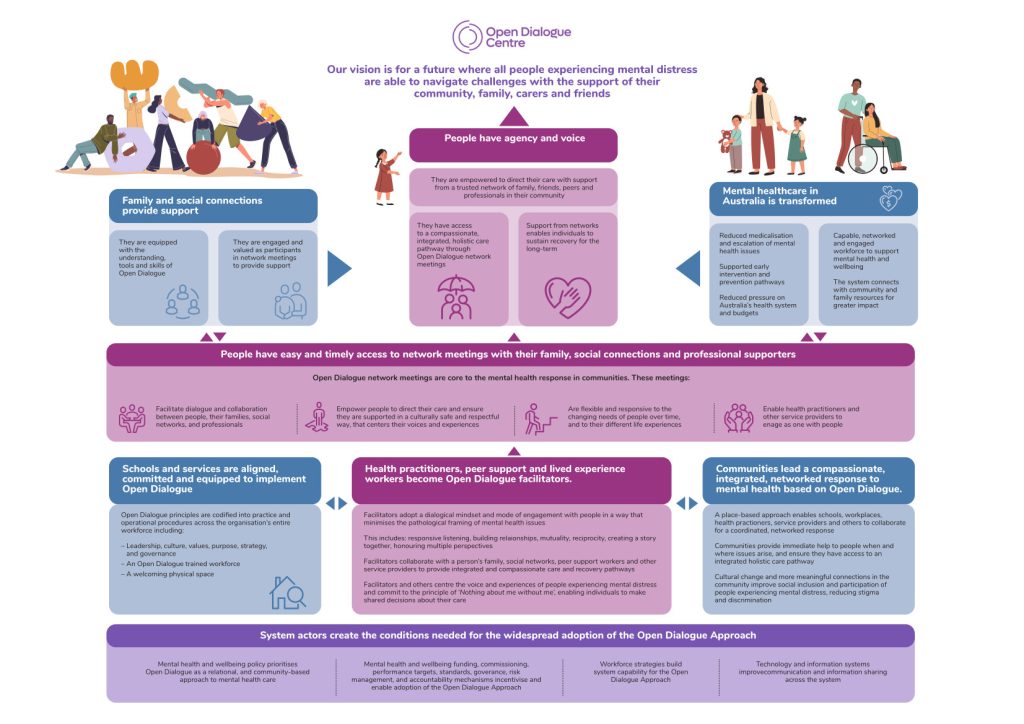
Please click on the image below to see a larger version of the Open Dialogue Centre Theory of Change.
Share this newsletter with a friend or colleague who you think will be interested in learning more about the shift towards community-led change in mental health